What Does Patient Engagement Really Mean?
We often hear terms such as patient engagement and they become the latest “term du jour”. But what does that really mean and what is your organization doing to help promote such activity? Is patient engagement a part of your organization’s strategy to maintain customer loyalty and grow your business?
Patient engagement is much more than just offering a portal or app that your patients can use to schedule appointments or see their latest EOBs. Patient engagement is more about a philosophy – a way that your organization will interact with your patients or members. This interaction needs to be bi-directional. Providing your patients with access to their health information may also be a part of this strategy. However, patient access to their data is not enough. What is critical is the need to help patients by engaging them and making sure they understand what their data is “telling” them.
The idea is to provide patients with the necessary information, guiding them and ensuring they are engaged with their own care, and making the right choices. This will lead to better outcomes and ultimately to a lower cost of care. This level of engagement requires that providers are active participants. By gaining a holistic view of the patient, then you, the provider, will become an active partner in the patient’s care. The need to run duplicative tests can be avoided. The ability to remind patients if they miss a prescription refill will help in establishing your organization as a trusted partner in the patient’s care. Some patients will obviously be more active participants than others, but if you are able to provide them with things like educational resources or support groups – this can also lead to a richer experience for the patient. The result – they will view your organization as their trusted source for their health needs.
Patient engagement requires patient data
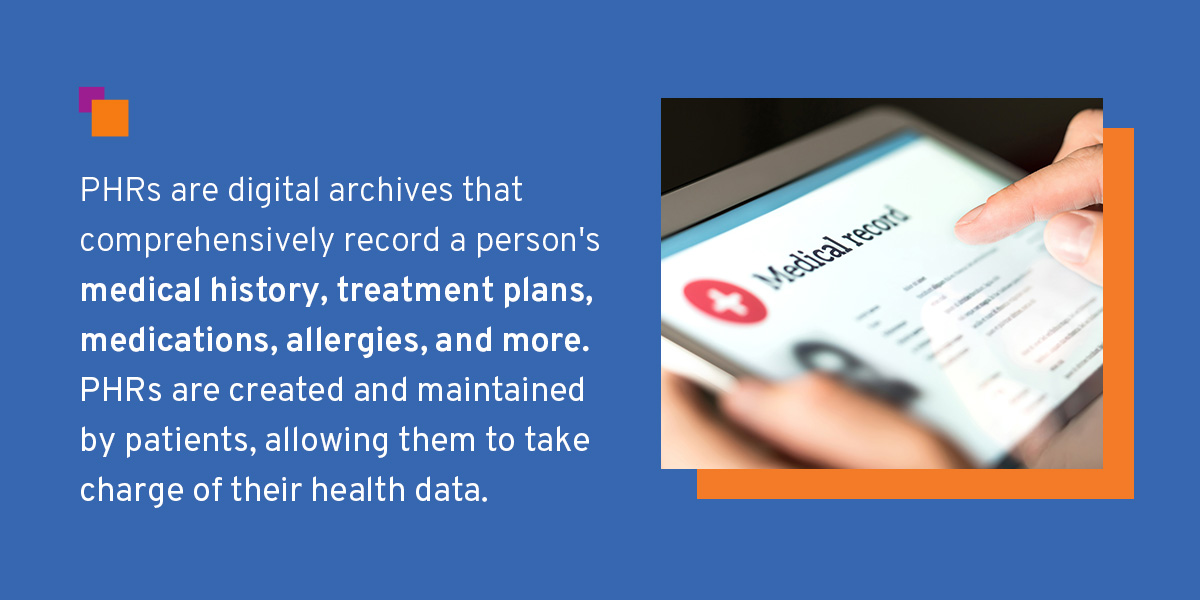
In our “information everywhere” world, patients can be easily overwhelmed with data. In today’s technology invasive environment, with wearables and the many health apps that are designed to help us, how do we make sense of it all? The need to pull together the many sources of data available to us as providers or as patients is leading to the advent of yet another enabling technology – the personal health record. The idea of a personal health record is not necessarily new, but we now see various technology companies, foundations, pharmaceutical companies as well as payers contributing to the personal health record, making it easier for the patient to truly be at the center of their care. These technologies are more user friendly to the patient and the provider. These applications make it easier to both collect and transmit personal health records, which when fully aggregated, can lead to greater insights for care management. They should also be particularly useful to everyone concerned with chronic disease management.
The bottom-line?
As a member of the health care ecosystem, the question you now need to ask is how will I engage and bring further value to my patient? What technologies can I enable for my patients to make true patient engagement a reality for my patients?
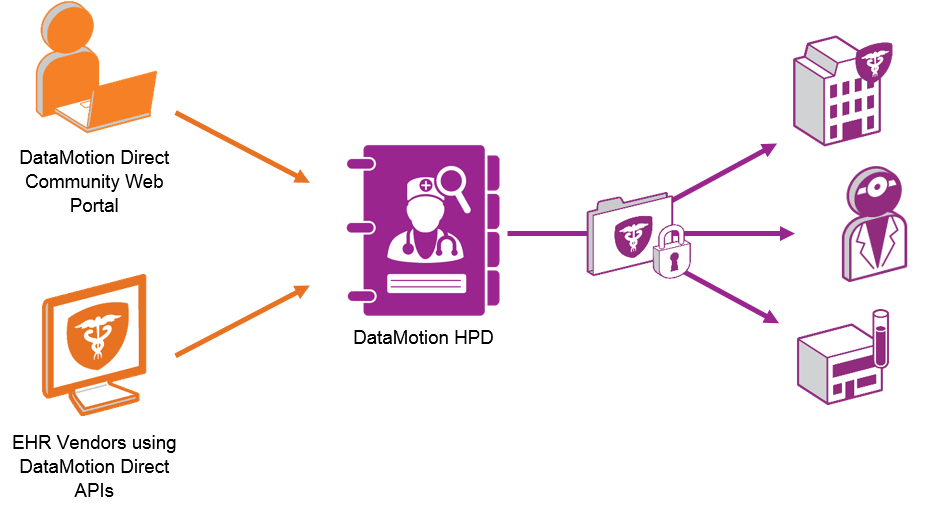
We believe that as this push for greater visibility and data access grows, DataMotion is well positioned to be the conduit for much of this communication flow.
How did one organization use DataMotion Direct Secure Messaging to improve care coordination, provider satisfaction, and CMS quality metrics?