Continuity, Connected.
How health plans can meet AHIP & BCBSA’s 2026 prior-authorization commitments securely, simply, and on time.
The nation’s leading health plans have pledged to simplify prior authorization for 260 million members — and the first milestone arrives January 1, 2026. Here’s how to get ready.

What Health Plans Need to Know About AHIP’s Prior Authorization Reform
Beginning January 1, 2026, participating plans must honor existing prior authorizations for a 90-day transition period when members switch coverage.
Prepare for the 2026 Continuity of Care Commitment Using Direct Secure Messaging
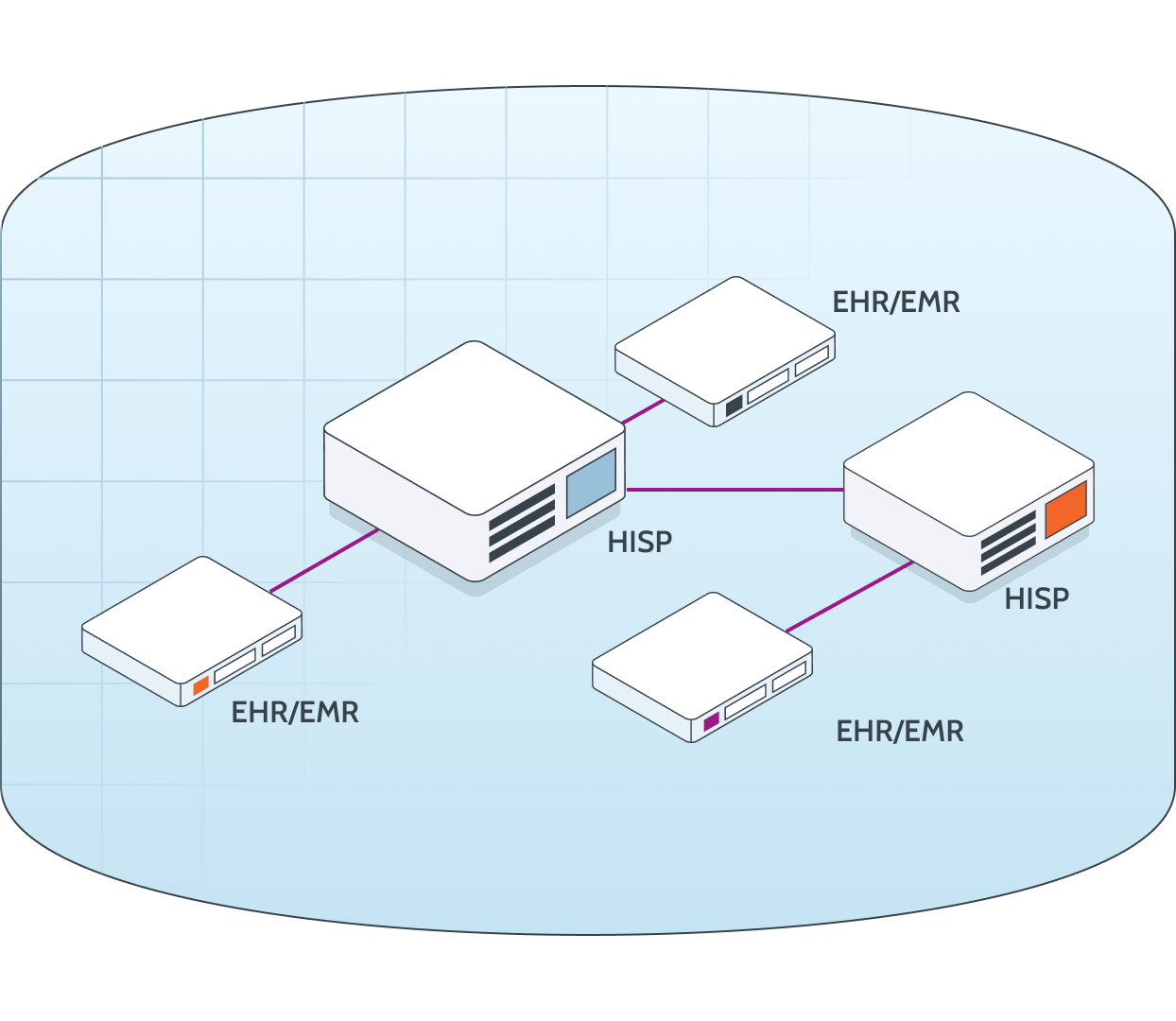
What Exactly is a HISP?
What is Direct Secure Messaging?
Health Plans Take Action to Simplify Prior Authorization
The 2026-2027 Prior Authorization Commitments
In June 2025, major U.S. health plans — representing more than 257 million covered members — signed a voluntary pledge through AHIP and BCBSA to simplify and accelerate prior authorization (PA).
The initiative spans both commercial and government markets and sets firm milestones for 2026 and 2027.
By January 1, 2026
- Reduce the Scope: Fewer services requiring PA by January 1, 2026.
- Ensure Continuity: Honor existing PAs for 90 days.
By End of 2026
- Clarify Decisions: Plain-language determinations and appeal steps.
By January 1, 2027
- Standardize Electronic PA: Adopt FHIR® APIs.
By End of 2027
- Expand Real-Time Approvals: 80% of complete requests answered instantly.
Ongoing
- Maintain Clinical Review: All denials reviewed by medical professionals.
Why This Matters for Health Plans
These commitments are voluntary but highly visible — participation and progress will be tracked publicly by AHIP and BCBSA.
That means payer organizations must demonstrate real action ahead of 2026.
However, the 90-day continuity rule is limited to active treatments, in-network providers, and benefit-equivalent services.
At the same time, FHIR infrastructure and real-time PA processing won’t be fully in place until 2027.
For many health plans, this creates a one-year gap between policy expectations and technology readiness — a gap that must be bridged securely and efficiently to avoid care delays.
Bottom line: The clock is ticking. Plans need a proven method to share PA data before the FHIR future arrives.
From Policy to Practice: How DataMotion Bridges the Gap
We’re the DirectTrust-accredited HISP enabling secure payer-to-payer exchange so health plans can honor prior authorizations and protect continuity of care — today.
Health plans need a fast, compliant way to honor existing prior authorizations before new API infrastructure is fully in place.
As a DirectTrust-accredited Health Information Service Provider (HISP), DataMotion delivers that bridge — enabling secure, standards-based exchange of prior authorization data today, while preparing for tomorrow’s FHIR®-driven workflows.
Secure Exchange
FHIR-ready architecture, DirectTrust network.
Fast Implementation
Deploy in weeks, not months.
Compliance Guaranteed
HITRUST CSF®, HIPAA-aligned.
Workflow Automation
Smart Secure Forms & APIs.
Future-Proof
Bridge now, seamlessly evolve to FHIR in 2027.
Trusted Partner
Proven in healthcare and financial services.
How DataMotion Helps
- Secure Payer-to-Payer Exchange: HIPAA-compliant transport layer using Direct Secure Messaging — no portals, no faxes, no delays.
- FHIR®-Ready Interoperability: API-friendly architecture aligned with CMS 2027 mandates, connecting Direct standards with API automation for continuous workflows.
- Low-Disruption Deployment: Integrates with existing systems, enabling health plans to demonstrate compliance before the 2026 continuity deadline.
Bridging the Gap Between Today and FHIR®
While FHIR® APIs will eventually standardize prior authorization, the 2026 continuity-of-care requirement demands a solution that works now.
Direct Secure Messaging provides an established, HIPAA-compliant pathway for payer-to-payer data exchange — without waiting for new API deployments or costly infrastructure builds.
As a DirectTrust-accredited HISP, DataMotion offers a proven framework to securely transfer PA documents, support traceability, and maintain full compliance with federal interoperability standards.
Think of it as the bridge from 2025 readiness to 2027 interoperability — secure, scalable, and ready today.

“You can’t wait for FHIR — and with DataMotion, you won’t have to.”
Andrew McKenna, VP of Product at DataMotion
Schedule a Readiness Consultation
Assess your continuity compliance before January 1.
Frequently Asked Questions
Is this new prior authorization reform mandatory?
No. The commitments are voluntary, but they are publicly tracked and represent plans covering more than 257 million members. Because the commitments are highly visible, many plans are treating them as expectations rather than optional participation.
What exactly changes on January 1, 2026?
Participating plans will begin honoring existing prior authorizations for 90 days when a member changes insurers, as long as the service is in-network and benefit-equivalent.
How does this relate to the 2027 CMS interoperability and FHIR® rule?
The AHIP/BCBSA commitments create a one-year readiness gap. Many plans will not have full FHIR® payer-to-payer APIs in place until January 1, 2027. Plans will need a secure interim solution to exchange prior authorization information in 2026.
What is a HISP and why is it relevant?
A Health Information Service Provider (HISP) enables secure, compliant exchange of clinical and administrative health information between organizations. HISPs—including DirectTrust-accredited HISPs like DataMotion—allow payer-to-payer exchange without waiting for new FHIR infrastructure.
Does this replace FHIR APIs or interoperability efforts?
No. HISPs provide a 2026-ready bridge to support secure exchange now, while plans continue building toward FHIR-based real-time prior authorization in 2027.
Can DataMotion help us exchange prior authorization documentation securely?
Yes. DataMotion enables secure payer-to-payer exchange using Direct Secure Messaging and FHIR-ready APIs to support continuity, traceability, and compliance.
How long does it take to implement?
Many plans can get live in weeks, not months, depending on existing infrastructure.
What types of documents can be exchanged?
PA documentation, clinical documents (CCD/C-CDA), PDF authorizations, supporting medical information, decision notices, and structured payloads supporting automation.
How do we get started?
Schedule a Continuity Readiness Consultation to evaluate your current capabilities and recommended onboarding path.
The Proof Is In The Numbers
-
2 KActive organizations
-
10 MActive users
-
32 %Support reduction
-
48 %Efficiency gain
✓ Secure.
✓ Compliant.
✓ Ready in Weeks.
The first milestone hits January 1, 2026. The question is — will your systems be ready?
Talk to Our Interoperability Team
"*" indicates required fields